February 5, 2024
2024 Physician Reimbursement Sustainability
- by Shannon DeConda, Partner, Founder and President of NAMAS
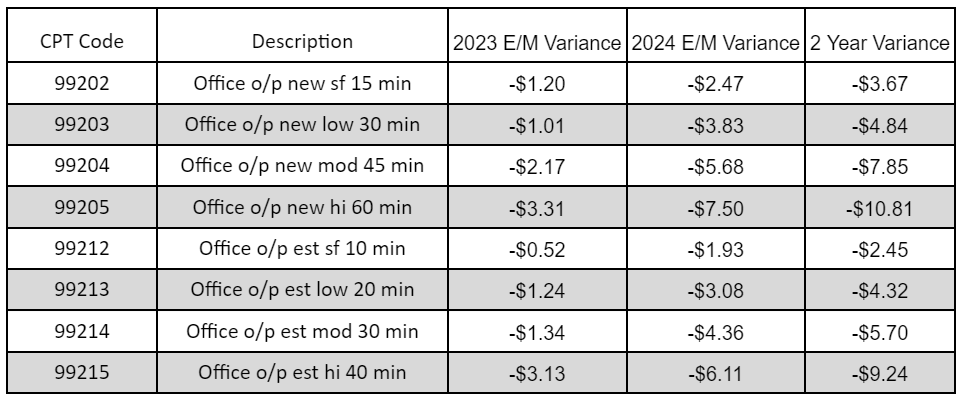
The year 2024 has brought in a notable decrease in physicians’ reimbursement rates. This is attributed to the adjustments made to the conversion factor used in computing the rates. These changes have significant implications for physicians, affecting their financial compensation for their medical services.
Reimbursement Reduction
Any business can feel the impact of reduced revenue, but the healthcare industry is particularly susceptible to its effects. However, the impact on the healthcare sector is not always completely considered. When the cost of consumer goods increases, a cheaper alternative can typically be found, or the purchase can often be delayed. When it comes to our health, delaying a choice is not always an option. Additionally, cheaper should not be our choice for our body and health, but furthermore, the patient doesn’t typically negotiate pricing when insurance is involved.
Physician practices, in particular, face unique challenges regarding revenue. Unlike a grocery store, Target, or your favorite designer brand, they do not have the ability to raise their rates because their overhead went up. They can’t raise their rates or balance bill their patients to offset their losses. Instead, they need to explore different service lines to generate new revenue. This can be challenging, but there are innovative new services that allow for concierge solutions to reimbursed patient care that can be implemented for new revenue streams.
Revenue Stream Viability
Adding service lines is a way to create revenue stream viability. As physicians navigate the dynamic healthcare landscape of 2024, the need to diversify revenue streams has become paramount. With evolving reimbursement models, technological advancements, and shifting patient preferences, physician practices must explore innovative strategies to ensure financial viability and long-term sustainability.
An example of using technology and staff to full capacity to leverage financial viability and create sustainability is implementing Chronic Care Management (CCM) services, which increase revenue and offer essential support to Medicare recipients with multiple chronic conditions. CCM provides non-face-to-face services that aim to enhance care coordination and improve patient outcomes, resulting in reduced healthcare costs. By prioritizing the complex needs of those with chronic illnesses, we believe healthcare providers can significantly impact their patients’ lives while finding revenue sustainability. To achieve this, a well-defined strategy and the right resources are crucial.
Viability of CCM as a Revenue Stream:
- Reimbursement: As a physician, you can receive consistent reimbursement for managing the care of eligible patients through CMS’s CCM services. These services offer financial incentives for providers to coordinate care, making it an attractive option.
- Expanded Care: By proactively managing patients’ health, physicians utilizing CCM can extend their care beyond episodic office visits, providing ongoing support and monitoring for those with chronic conditions. This approach can lead to improved outcomes, reduced hospitalizations, and increased patient satisfaction while generating revenue through CCM reimbursement.
- Practice Sustainability: Integrating CCM services into practice workflows can contribute to the long-term sustainability of physician practices. By diversifying revenue streams and focusing on proactive, value-based care, practices can better withstand financial uncertainties and adapt to evolving reimbursement models. This approach ensures patients receive the personalized care they need while helping practices stay financially stable.
Principle Care Management (PCM), the cousin to CCM, is a similar service. PCM mirrors the 3 concepts above and is typically used for patients needing additional support care management for approximately 6 months due to acute or chronic illness or exacerbation.
Minimize the Challenges
Implementing a new service is not typically an easy process. To get the most out of the CCM, PCM, or Transitional Care Management (TCM) (not discussed above), the process must be kept within the practice and not performed by a third party. Not only is it more financially beneficial, but your patients will certainly notice the difference in the level of care they receive.
- It is important to ensure that all staff members are properly trained on the requirements for CCM, documentation protocols, and billing procedures to provide effective delivery and support for these services. Do NOT shy away from creating appropriate documentation templates.
- Educating patients about the benefits of CCM services and encouraging their participation in care management activities can help optimize outcomes and ensure the viability of your CCM | PCM program. Engaging patients in their care is important to ensure they receive the best possible treatment.
- Establishing robust care coordination processes is essential to ensure seamless transitions and continuity of care among healthcare providers involved in the patient’s care. This involves facilitating communication and collaboration to ensure the patient’s unique goals and circumstances are considered and achieved. Your patients and other care partners will truly value your practice’s outstanding care coordination, helping build a positive and compassionate reputation.
Plan of Action
To get started, it’s important to have a plan of action. Consider selecting a “Team Captain” who is a motivated and task-focused individual, capable of overcoming obstacles without getting easily discouraged.
The following are noteworthy tasks to get you on your way:
- When creating consent forms for Chronic Care Management (CCM) and Patient Care Management (PCM), it may be helpful to consider using a template for the initial visit.
- It’s important to educate ancillary staff on their role in providing CCM services and education, and templates for required documentation can be useful.
- Additionally, physicians and providers should be educated on documentation requirements and the value of CCM for their patients.
- Billing and EMR setup should also be taken into consideration.
Other tasks are needed for complete and successful integration. Coaching and support are available from firms such as DoctorsManagement, but successful integration can be done by self-integration as well.
Consider downloading the DM CCM Resource Guide, which is full of useful information, and using the links provided throughout this blog.