May 24, 2024
Common HIPAA Compliance Violations in Healthcare
- by Shanon Moore, Director, OSHA/HIPAA Compliance
Protecting patient information is paramount in the ever-evolving healthcare industry. The Health Insurance Portability and Accountability Act of 1996 sets the standard for shielding sensitive patient data. However, despite stringent regulations, violations still occur — often due to oversights or misunderstandings.
HIPAA compliance is an ongoing journey for healthcare organizations requiring diligence, vigilance, and a commitment to safeguarding patient information. As a healthcare provider or entity, you must understand the common HIPAA violations and familiarize yourself with compliance requirements to mitigate compliance risks and safeguard your business.
Enforcement Results as of Jan. 31, 2024
Since the Privacy Rule’s compliance date in April 2003, the Office of Civil Rights has managed over 351,372 HIPAA complaints and conducted 1,183 compliance reviews. Nearly all cases — totaling 348,503 — have been effectively resolved.
The OCR has overseen the resolution of more than 30,675 cases, necessitating adjustments in privacy protocols and corrective measures by HIPAA-covered entities and their affiliates. Throughout this period, OCR has reached settlements or imposed civil penalties in 142 instances, amounting to approximately $142.5 million in penalties. The range of investigations has targeted various entities, including national pharmacy chains, major medical institutions, group health plans, hospital chains, and smaller provider offices.
The most commonly cited compliance issues, in descending order of frequency, include the following:
- Prohibited use and disclosure of protected health information.
- Inadequate safeguards for PHI.
- Patient PHI access limitations.
- Insufficient administrative safeguards for electronic PHI.
- Overuse or unnecessary disclosure of PHI.
Similarly, the types of covered entities most frequently implicated in violations include the following in descending order:
- General hospitals
- Private practices and physicians
- Pharmacies
- Outpatient facilities
- Community health centers
OCR remains steadfast in enforcing the HIPAA Privacy, Security, and Breach Notification Rules, mandating compliance for covered entities and their business associates to safeguard PHI and adhere to breach notification protocols.
Top 5 HIPAA Compliance Violations
Here, we will discuss the 5 most common HIPAA compliance violations in healthcare.
1. Unauthorized Use and Disclosure
Unauthorized use and disclosure describe situations in which organizations or healthcare professionals share or use patient PHI in ways not allowed by HIPAA standards.
This kind of breach can happen when someone discloses private data to unauthorized parties or organizations or uses it for reasons unrelated to medical treatment or without the patient’s consent. It covers circumstances in which medical personnel reveal patient data without authority or divulge more data than is necessary for a specific objective.
Such confidentiality violations may have detrimental effects on patients and healthcare professionals, including financial penalties, reputational harm, legal repercussions, and loss of confidence.
To avoid infractions, healthcare organizations must ensure all staff members receive sufficient training on HIPAA requirements and establish distinct policies and procedures governing the permitted uses and disclosures of PHI.
2. Lack of Safeguards
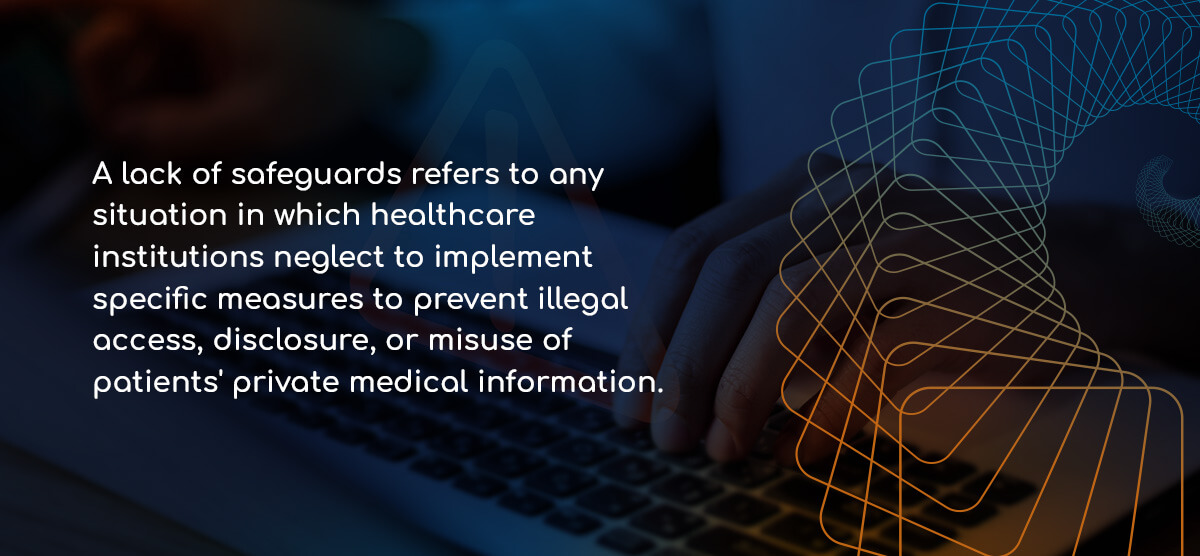
A lack of safeguards refers to any situation in which healthcare institutions neglect to implement specific measures to prevent illegal access, disclosure, or misuse of patients’ private medical information.
This violation often arises due to insufficient security protocols, such as weak password policies, lack of encryption for EHR, or inadequate physical security measures to safeguard paper records.
Consequently, patient data can become susceptible to security breaches, cyberattacks, or theft, posing significant risks to confidentiality and privacy. Without proper procedures in place, healthcare providers may inadvertently expose patients to identity theft, fraud, or discrimination based on their health status. Such lapses in data security may lead to regulatory penalties, legal liabilities, and damage to the organization’s reputation.
To reduce the risk of data breaches and guarantee compliance with HIPAA standards, healthcare organizations must prioritize installing security measures, such as access limits, encryption, frequent risk assessments, and staff training.
3. Lack of Patient Access to Health Information
Patients have the legal right to view PHI kept by covered entities, as per HIPAA regulations. Denying patients this access violates their privacy rights and impedes their ability to manage their healthcare effectively.
This violation may result from several things, including administrative hurdles, refusal to provide requested records, or excessive delays in fulfilling access requests. Failure to facilitate patient access undermines transparency in healthcare delivery and prevents patients from actively participating in their treatment decisions.
4. Lack of Administrative Safeguards for ePHI
The HIPAA compliance violation refers to the failure to implement policies and procedures to protect EHRs.
These include inadequate steps to ensure the confidentiality, integrity, and availability of ePHI. Common examples include insufficient access controls, weak password policies, and incomplete employee training on data security protocols. Such oversights may lead to unauthorized access, data breaches, and compromise of patient privacy.
Healthcare organizations must establish robust administrative safeguards to mitigate risks associated with ePHI. These safeguards should include risk assessments, regular audits, and implementing security measures aligned with HIPAA regulations.
5. Excessive Use or Disclosure of Patient Information
The excessive use or disclosure of PHI refers to situations where healthcare entities share or access more patient data than is required for a particular purpose. HIPAA mandates that healthcare providers limit the use or disclosure of PHI to the minimum necessary to accomplish the intended aims.
This violation occurs when entities fail to apply this principle, potentially compromising patient privacy. For example, sharing unnecessary details with unauthorized personnel or accessing more information than needed for treatment can lead to this violation. It undermines patient confidentiality and increases the risk of unauthorized access or exposure to sensitive health data.
Healthcare organizations must implement strict policies and procedures around accessing and disclosing essential PHI to minimize the risk of this violation.
What Are the Penalties for HIPAA Violations?
Violating HIPAA carries significant consequences. Even in instances of unintentional HIPAA violations, the consequences can be severe.
Civil Violations and Penalties
Civil penalties are usually part of cases where the offender was unaware they were committing a HIPAA violation. The civil penalty structure uses four categories based on the level of culpability, with the penalty limit for each tier being $2,067,813 annually.
The four categories are as follows:
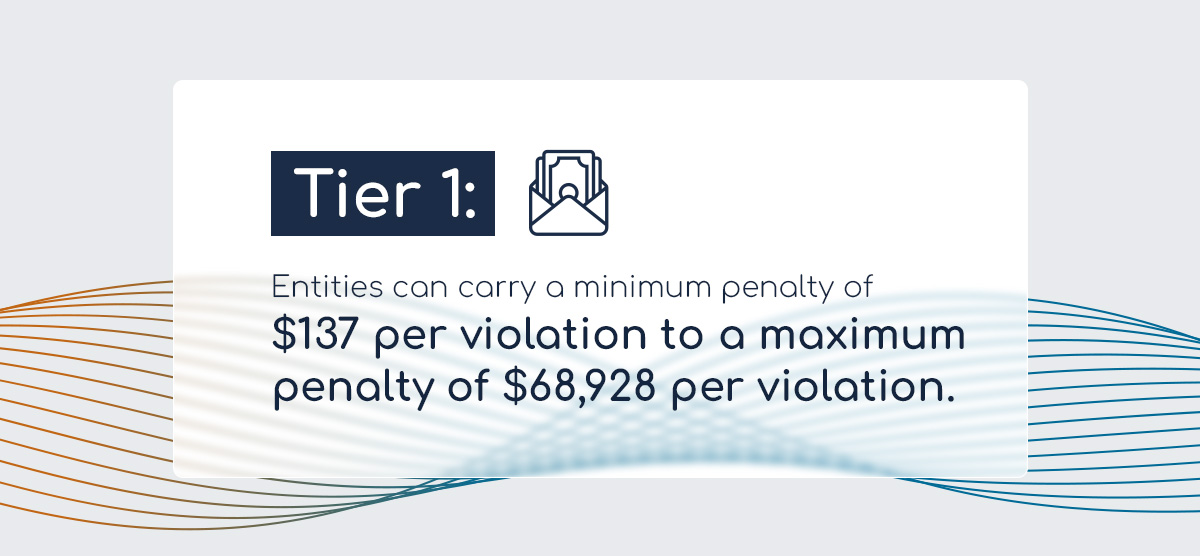
- Tier 1: The entity had a lack of knowledge. Entities can carry a minimum penalty of $137 per violation to a maximum penalty of $68,928 per violation.
- Tier 2: An infraction that the entity should have recognized but could not avert — a reasonable cause. Entities can carry a minimum penalty of $1,379 per violation to a maximum penalty of $68,928 per violation.
- Tier 3: The entity willfully neglects HIPAA rules — however, the entity corrected it afterward. Entities can be penalized by a minimum of $13,785 per violation to a maximum of $68,928 per violation.
- Tier 4: The entity willfully neglects HIPAA rules and does not correct them within 30 days. Entities can be penalized by a minimum of $68,928 per violation to a maximum of $2,067,813 per violation.
Criminal Violations and Penalties
Criminal penalties are usually issued in cases where people knowingly obtain or use PHI without permission, and those violations and penalties fall under three tiers.
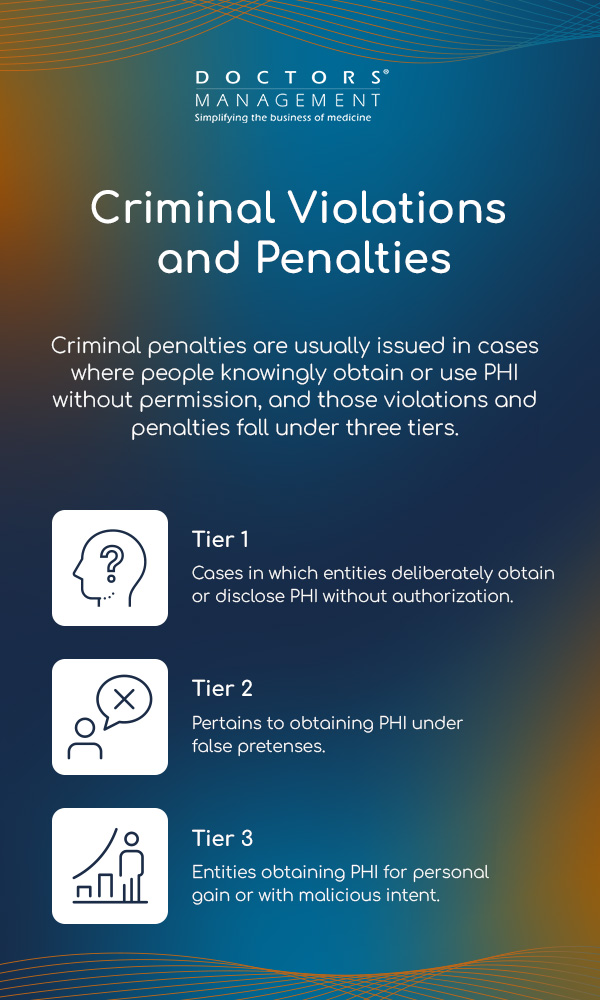
The three tiers are as follows:
- Tier 1: Cases in which entities deliberately obtain or disclose PHI without authorization can result in a penalty of up to one year in jail and a $50,000 fine.
- Tier 2: Entities obtaining PHI under false pretenses can result in a penalty of up to five years in jail and a $100,000 fine.
- Tier 3: Entities obtaining PHI for personal gain or with malicious intent can result in a penalty of up to 10 years in jail and a $250,000 fine.
OCR refers appropriate cases to the Department of Justice for criminal investigation involving the knowing disclosure or obtaining of PHI violating the rules. As of Jan. 31, 2024, OCR had made 2,074 referrals to the DOJ.
How Can I Prevent HIPAA Violations?
Healthcare providers can follow these guidelines to uphold patient data integrity and ensure compliance with HIPAA regulations.
Regular Staff Training
HIPAA requires that covered entities and business associates provide HIPAA training to members of their workforce who handle PHI. The Privacy and Security Rules provide training requirements for security reminders, the handling of PHI, and documentation of this training. Employees should initially complete training on the practice’s policies and procedures with respect to PHI.
Additionally, periodic refresher training should be an ongoing part of regular operations to ensure a culture of compliance and awareness. These courses can reinforce knowledge and highlight regulation updates or changes.
Routine Security Risk Analysis
Regularly conducting comprehensive risk assessments and audits helps identify vulnerabilities and gaps in security protocols. These assessments should cover all systems, processes, and policies for handling PHI. Providers must continuously monitor and evaluate these measures’ effectiveness to maintain a proactive stance against potential violations.
Ensuring Patient Access
Healthcare providers must not refuse patients access to their medical records or exceed the allowed time frame for providing these records. Patients have a right to access copies of their PHI, amend or update their information, account for all disclosures, and trust that the practice will transmit PHI with the appropriate restrictions and safeguards. Denying access or delaying records beyond the permitted 30 calendar days violates HIPAA regulations.
Administrative Safeguards of ePHI
The HIPAA Security Rule defines administrative safeguards as actions policies and procedures aimed at overseeing security measures, safeguarding ePHI, and instructing the behavior of the covered entity’s staff to ensure the protection of such data.
The standards included in administrative safeguards are high-level objectives and include the following:
- Security management processes
- Assigned security responsibility
- Workforce security
- Information access management
- Security awareness and training
- Security incident procedures
- Contingency plans
- Evaluation
- Business associate agreements
Minimum Necessary Requirement
The minimum necessary standard is a key protection of the Privacy Rule and should be common practice. This rule requires covered entities to evaluate their practices and enhance safeguards as needed to limit unnecessary or inappropriate access to and disclosure of health information. The fundamental principle is that health providers should not use or disclose PHI when it is not necessary to satisfy a particular purpose or carry out a function.
HIPAA Compliance Solutions From DoctorsManagement
Adhering to HIPAA rules and regulations is fundamental for healthcare organizations to protect their patients and themselves. HIPAA compliance demands unwavering commitment and continuous improvement from healthcare organizations.
DoctorsManagement offers tailored HIPAA compliance services to guide healthcare practices through these constantly changing times. Our compliance consultants ensure your practice understands the HIPAA rules and regulations and excels in implementing policies and procedures that seamlessly align with these requirements.
Please get in touch with us for a free consultation today.